
The RSQ® Solutions – Emergency Medicine Assessment is a retrospective chart review tool providing a granular analysis on physician practice patterns. The online tool focuses on the 10 highest risk chief complaints in emergency medicine and measures clinical alignment around best practice and documentation compliance with these high-risk patients.
What does the Assessment Tool measure?
The Emergency Medicine Assessment measures clinical practice and documentation. What did the physician do at the bedside clinically? Even if it was done clinically, was it documented? If an item is not documented in the chart, we have to assume the item wasn’t clinically performed. If the chart as the legal document doesn’t reflect the clinical action, the chart is vulnerable.
The Assessment Tool uses a proprietary metric called the RSQ® Score to determine a physician’s Risk, Safety and Quality profile. Indicators represent the most critical information needed to catch the most frequently missed high-risk diagnoses. If you don’t consistently gather all the RSQ® Score clinical indicators, you’re more exposed to missing diagnoses. The more consistently you gather all the RSQ® Score clinical indicators, the more likely you are to catch high-risk diagnoses. If you do miss a diagnosis, it’s more difficult to bring litigation against you because the indicators help create a more complete and defensible medical record. Improvements in RSQ® Score have correlated to a reduction in missed and delayed diagnosis malpractice claims.
Why use the Assessment Tool?
While education creates a knowledge foundation, it only validates an individual’s understanding of content. The assessment tool measures whether this best practice knowledge is being implemented at the bedside. Using the two simultaneously creates an effective, proactive approach to changing clinical practice and preventing adverse events and malpractice claims.
As a medical leader, you want your physicians aligning with best practice, especially with high-risk patients. While reducing variability in care is likely a priority, nowhere is it more important than in the most frequently missed diagnoses that can lead to adverse events in your facility. To achieve clinical alignment, it is critical to measure each physician’s individual practice. The assessment tool conducts a granular analysis to see how each physician is doing compared against a standard RSQ® (risk, safety, quality) Score.
With this detailed analysis, you can align physicians more closely clinically so they work up patients in a similar way. This clinical alignment helps reduce the likelihood of missing high-risk diagnoses that lead to adverse events and the likelihood of being on the receiving end of a lawsuit.
Additionally, use of the Emergency Medicine Assessment Tool satisfies the American Board of Emergency Medicine’s recertification requirements.
How does it work?
Assessment Planning Process
As the administrator of the program, a medical director will first define the targeted chief complaints and the number of charts to be entered for each chief complaint per physician over a given period. There are ten chief complaint audits available aligning to the 15 most commonly missed diagnosis-related claims in emergency medicine:
|
High-Risk Clinical Entities |
Failure to Diagnose/Treat |
|
Abdominal Pain Over 40 Years Old |
AAA, Appendicitis |
|
Chest Pain Over 30 Years Old |
AMI, PE, TAD |
|
Children with Fever |
Meningitis |
|
C-Spine Injury |
SCIWORA |
|
Extremity Laceration |
Foreign Body, Tendon Injury |
|
Fracture |
Fracture |
|
General Abdominal Pain |
Appendicitis, Torsion, Ectopic Pregnancy |
|
Headache |
SAH |
|
Head Injury |
Neurologic Impairment |
|
Vaginal Bleeding |
Ectopic Pregnancy |
As a best practice, we recommend starting with:
- 5 chief complaints. Choose any in which you might have recently experienced an adverse event or close call. Ask your risk management team which areas have produced the most claims in recent history.
- 10 charts for each chief complaint per physician.
With this foundation, an administrator has the autonomy to modify the following elements in subsequent review cycles:
- The review period
- The targeted chief complaints
- The number of charts entered for each chief complaint
Data Abstraction Process & Resources
The online assessment tool requires the abstraction of data from the medical record into the online tool. We recommend allocating a team of reviewers (1-2 reviewers per facility) to review data from the existing medical record and input online. The Sullivan Group provides training to reviewers regarding what to look for and best practices of review.
Recommended First-Year Schedule
Assuming a January 1 program start date, the following is a best practice schedule we recommend to capitalize on the data and insights available from this assessment tool.
1st Quarter
- Reviewer training
- February - March – Chart entry into assessment tool
2nd Quarter
- Generate reports
- Analyze for trends & insights
- Create an action plan to address vulnerabilities
- Share assessment results & action plan with staff (at a department meeting)
3rd Quarter
- Chart entry
4th Quarter
- Re-evaluate results and report back on Q2 action plan impact
Reports available to leadership
Once the data is entered, leadership has access to a dashboard through which reports can be generated to show where the hospital and the clinical staff are exposed to potential adverse events and litigation. Available reports include:
- Overall Risk & Quality Summary at a Glance
- Physician Reports
- Overall Physician Risk Profile by chief complaint
- Physician performance by phase in the process of care (history taking, discharge process, etc.)
- Department performance on clinical indicators by Chief Complaint (e.g., Is your department struggling with documenting radiation of pain in chest pain patients?)
- Compare performance of providers across the department by chief complaint
- Individual provider performance by chief complaint provides transparency into potential exposure (e.g., What is this individual missing?)
- Nursing Reports
- Overall Nurse Risk Score by chief complaint
- Nurse performance by phase in process of care (risk assessment, patient management, etc.)
- Department performance on clinical indicators by Chief Complaint (e.g., Ordering ECG within 10 minutes for chest pain patients?)
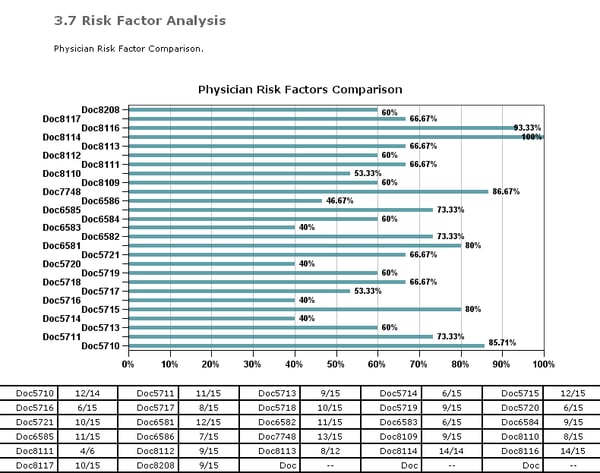
The ultimate target is to reduce variability in care. The goal isn’t “cookie cutter” medicine, but a closer alignment between providers. See the sample graph below for an example. In a department full of board-certified physicians, there shouldn’t be a 60% variance in the completion of a risk factor analysis. Reducing variability leads to a reduction in the likelihood of an error or adverse event.
What kind of action plans frequently come out of use of the assessment tool?
After each review cycle, leadership should analyze reports and create an action plan to address the vulnerabilities identified.
Based on risk exposures, the facility and The Sullivan Group work together to implement corrective action plans for performance improvements. For example, is your organization inappropriately discharging patients with abnormal vital signs? What’s the best solution to remedy this problem?
Some organizations identify that a change needs to be made to the medical record to collect a new field of data or move another field to a different area of the physician’s workflow to ensure its collection. For example, if physicians aren’t consistently addressing risk factors, let’s work to get those added to your medical record. When prompted by the EMR, they are more likely to collect this important data point.
Other concerns might be addressed with prioritizing certain education. If physicians aren’t documenting meningeal signs, an organization might choose to add a Pediatrics Meningitis course to next quarter’s education requirements.
How much does it cost to license the Emergency Medicine Assessment?
RSQ® Solutions – Emergency Medicine Assessment Pricing:
$.50/ED Visit for 5 chief complaints; $.65/ED visit for 10 chief complaints
For example:
- 20,000 Annual ED Visits & 5 chief complaints = $10,000/year license fee for 3 years
- 20,000 Annual ED Visits & 10 chief complaints = $13,000/year license fee for 3 years


