
[4 MIN READ]
Every patient – regardless of the time of day or department to which they present – needs to encounter a high-quality experience. Improving patient experience and ensuring its consistency involves reducing the variability between departments, clinicians and shifts.
To achieve this high goal, you need to get buy-in from the entire clinical community – an effort led by clinicians for clinicians to help all truly understand and buy into the mission and purpose of providing a high-quality patient experience.
Using the industry analyses to galvanize organizational support for defining a provider-patient communication model is a great first step. However, building an evidence-based training standard that improves outcomes (HCAHPS) and maintains clinician support (participation) is the next critical step. Through our experience with Dr. Doug Finefrock, we outlined a strategy to build a provider-patient communication training program that followed a specific criterion:
- Evidence-based, to the extent possible
- Systematic and scalable across large organizations
- Clinician-led and specific to healthcare
- Sustainable and objective
- Outcomes-based, to the extent possible
Based on these parameters, the steps below outline the critical practices necessary to provide the consistency and tools clinicians can use to improve their communication with patients.
Step 1 - What do patients want?
Before we can develop a system to impact patient experience, we first need to understand what patients want out of their experience. In a recent study, Finefrock et al.1 outline a subset of patient-centered communication behaviors correlate with higher patient satisfaction scores. Based on this feedback, we can define phases of the patient encounter and teach best practices in each.
Step 2 – Initial Evaluation
It is important to gather a baseline assessment of how your clinicians currently interact with patients before stepping into a training program. Conducting an initial performance assessment allows you to measure how well knowledge is applied at the bedside and how each individual clinician is improving.
Step 3 – Online Training
Deploy an online training program to teach the best practices defined above. Effective training should be video-based and rooted in the core adult learning concepts to keep learners engaged and interested. It is helpful to provide CME or CE credit for the exercises to boost participation.
Ideally, your education addresses all clinic and hospital staff that have potential to impact the patient experience, including physicians, mid-level providers, nurses and other healthcare employees in both the hospital and office settings.
For example, our PatientSET™ Education for nurses steps through several pertinent HCAHPS scenarios and outlines poor and best practices to learn from.
For physicians, we focus on the most common malpractice scenarios, demonstrating how poor communication leads to errors. This approach grabs the attention of physicians because the scenarios are relevant and timely.
Education for other healthcare employees focuses on healthcare-related customer service principles. How well are they answering the phone, whether it’s hospital staff or a patient? How are patients greeted?
Step 4 – Re-Assessment Against List of Best Practices
How well are your clinicians applying their new communication skills at the bedside? Deploy an observational assessment after training to measure performance improvements and opportunities for improvement.
Step 5 – Objective Action Plan
Based on how well behaviors are performed on re-assessment, management can put together an objective action plan to guide each clinician’s performance improvement strategy. Give examples of what someone is doing well and where they can improve.
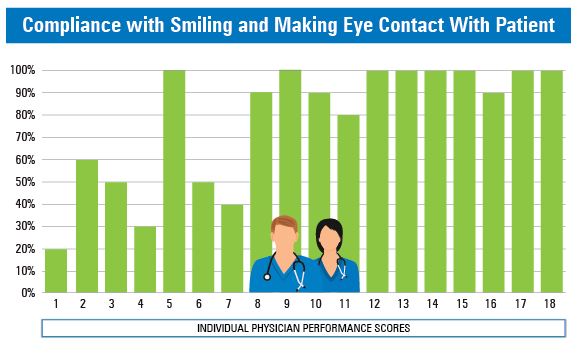
Clinicians tend to be competitive and relate to objective measures comparing their performance to others in their peer group. Management can strategically use reporting metrics to identify how a physician is performing on specific best practices. For example, one physician who never smiles and makes eye contact is performing poorly on this measure related to peers. This grabs a physician’s attention and can consequently affect change.
Step 6 – Re-Evaluate Annually
Provide a training review each year and a re-assessment to gauge improvements.
Step 7 – Celebrate Successes
Share departmental or individual improvements and good reviews with the team periodically in meetings to keep positive momentum and morale.
Summary
As you evaluate whether you might design your own program to improve patient experience, use the following evidence-based criteria:
- The program should be scalable and reproducible across a large organization.
- Include an ongoing performance evaluation through an observational performance assessment.
- Create an objective action plan based on personal performance.
- Use an outcome-based evaluation to drive measurable improvements.
It is impossible to create a high-quality patient experience without creating a foundation that focuses on a consistent provider-patient communication model – one that creates a great first impression, manages expectations, and clearly communicates at discharge. A program designed in this manner reduces variability in the patient experience across your organization.


