A 35-year-old female presents at 0321 by ambulance with a complaint of chest pain. The records show EMS arriving at her house and finding the patient on the couch.
A 35-year-old female presents at 0321 by ambulance with a complaint of chest pain. The records show EMS arriving at her house and finding the patient on the couch.
EMT Notes
Patient appears to be anxious and hyperventilating. Encouraged patient to slow breathing down. VS obtained: Pulse 120; BP 152/112; Resp. 22, shallow. Patient complains of: intermittent sharp chest pain located in sternum area non-radiating; started at 0230. Pain is 8 on a scale of 1-10. Patient also complains of an increase in pain upon palpation to the sternum and with coughing. Patient has a productive cough of a clear, thick substance. Denies fever or recent trauma. Patient states she has had the chills for the past week. Lung sounds are clear and present in all lobes excluding the left lower lobe, which is diminished. Abdomen soft non-tender. Further exam unremarkable.
 The EMT started an IV and administered NTG x 3, but no improvement was noted. He then administered Morphine Sulfate 2 mg IVP x 3 per protocol, and the pain decreased to a 6.
The EMT started an IV and administered NTG x 3, but no improvement was noted. He then administered Morphine Sulfate 2 mg IVP x 3 per protocol, and the pain decreased to a 6.
EMT Impression
- R/O chest wall pain, pleuritic pain
- R/O cardiac chest pain
- R/O pneumonia, upper respiratory infection
- R/O PE
Nursing Triage Note
The triage is timed 0321. The triage nurse noted: chest pain, productive cough. Started 1 week ago, has just worsened. Has chills and cough. PMH: HTN and CVA. EMS Meds 4 ASA, 3 NTG. Meds include: amlodipine, atenolol, nortriptyline, desloratadine, escitalopram, tizanidine, sumatriptan, hydrocodone.
Triage Vitals (timed 0230): Pulse 97, BP 142/115, Resp 14, Temp 97.2°F (36.2°C), SpO2 98%, Pain 8/10.
The physician saw the patient at 0348; he documented his exam on an electronic medical record using a chest pain template.
History of Present Illness
| Chief Compliant | Chest Pain |
| Started | Awakened her 0250 |
| Time Course | Still present; constant |
| Quality | Pressure, tightness, sharp |
| Location of Pain | The sternal area is circled on the body illustration. |
| Radiation | This section was not filled in; radiation was not addressed. |
| Associated Symptoms | Nausea, shortness of breath and sweating; no vomiting |
| Worsened by | Deep breath |
| Relieved by | Nitroglycerin x 3 by paramedics and MS gave partial relief; oxygen |
| Onset During | Sleep |
| Pain Severity | Severe |
| Pain When Seen in ED | The physician noted "recurring," without a number. |
| Similar Symptoms Previously | 2 episodes, brief, this past week |
ROS
Positive for occasional cough, headache. Negative for fever, ankle swelling, leg pain, blackouts, abdominal pain, black stools, problems urinating, skin rash, joint pain. All systems neg. except as marked or checked.
PMH
High blood pressure, gestational diabetes, chronic bronchitis, CVA three years ago, migraines. PMH negative for high cholesterol, heart disease, DVT risk factors, peptic ulcer and gallstones.
Allergies: No known allergies
Social History: Negative
Family History: Negative for CAD. Positive for lung cancer, epilepsy and diabetes.
Physical Exam:
| General | Appears anxious. She is holding her chest. |
| HEENT | Checked as normal on the template |
| Neck | Checked as normal on the template |
| Respiratory | Checked as normal on the template |
| CV | Regular rate and rhythm, no murmur, no gallop, no rub |
| Chest | Mild chest wall tenderness, left side, mid clavicular line |
| Abdomen | Checked as normal on the template |
The skin, extremities, neurologic and mental status exam were also documented as normal.
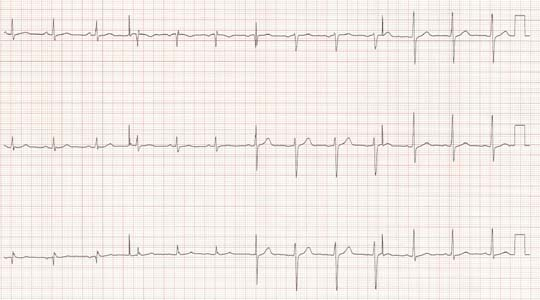
The ECG, which the physician interpreted as normal, is shown below:
ED Course
The physician ordered the ED acute chest pain protocol, which included:
- Oxygen 2L/min by nasal canula
- IV 0.9 normal saline at 125 ml/hr
- Chest X-ray
- Aspirin 325 mg PO
- Morphine Sulfate 2mg IV PRN titrate to pain
- Metoprolol 5 mg IV slow q 5 minutes x3, or until HR 50-60 and SBP> 90
- Basic Metabolic Profile, BMP, troponin, CBC
- ECG on arrival and at 1 hour
The initial chest X-ray was interpreted as normal by the emergency physician, who noted, "no infiltrates, normal heart size." Her Pulse Ox was 98%-99% on room air. Her electrolytes, CBC, and BMP were all within normal limits; troponin was 0.05 (reported as normal for this hospital).
Nursing Progress Notes
| 0425 | Morphine 2 mg IVP. Pain 8/10. Vitals: Pulse 84, BP 142/92, Resp 20. |
| 0435 | Toradol 60 mg IM. |
| 0545 | The patient was discharged home. |
Patient Discharge
| Physician Impression | Left-sided chest wall pain, musculoskeletal |
| Discharge Instructions | Warm pack to chest wall |
| Prescription | Naproxen and acetaminophen/hydrocodone |
| Follow-Up | None |
| Discharge Vital Signs | Pulse 76, BP 107/69, Resp 14, Pain 6/10 |
Outcome
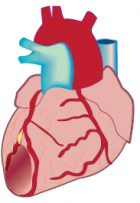
Eleven days later, the patient presented to the same ED in full cardiac arrest. Autopsy revealed a 95% atherosclerotic narrowing of the LAD.
Following the depositions with the physician and nurses, the defendants settled out of court with the patient’s family for an undisclosed amount.
Case Discussion
- Rule Out MI. On the patient’s arrival, the physician appropriately considered the possibility of acute coronary syndrome. However, he did not continue management to rule out the disease. This patient had chest pain, risk factors for coronary artery disease, and known prior cerebrovascular disease. The physician applied a faulty thought process as he anchored on the presence of reproducible chest wall pain and in determining that he had ruled out an acute coronary syndrome.
- The Second ECG. The physician ordered but never obtained a second ECG. The first ECG does appear normal, as the emergency physician noted. However, the failure to obtain a second ECG at one hour was one of the major allegations against the physician, nurses and the hospital.
 Troponin Timing. On arrival in the ED, the pain had been present for less than two hours. The patient reported the onset of pain occurred at 0230. Labs were drawn soon after arrival in the ED. Troponin is not present in the serum until three hours after the onset of pain; it is present at 3 hours and peaks at 12 hours. It is not possible to rule out acute coronary syndrome with one troponin test at the two-hour mark. This is a common finding in failure to diagnose MI cases. The inappropriate use of cardiac markers is a significant and recurring issue.
Troponin Timing. On arrival in the ED, the pain had been present for less than two hours. The patient reported the onset of pain occurred at 0230. Labs were drawn soon after arrival in the ED. Troponin is not present in the serum until three hours after the onset of pain; it is present at 3 hours and peaks at 12 hours. It is not possible to rule out acute coronary syndrome with one troponin test at the two-hour mark. This is a common finding in failure to diagnose MI cases. The inappropriate use of cardiac markers is a significant and recurring issue.- Atypical Presentation of Acute Ischemic Heart Disease in Women. This presentation clearly has some atypical components for acute MI or unstable angina. See the lists below of this patient’s typical and atypical signs and symptoms abstracted from all the notes.
Ischemic heart disease is underdiagnosed in women. Look at the list of typical signs/symptoms; there is no way to rule out acute ischemic heart disease based on these elements of the history and physical and a single troponin and ECG.
| Atypical | Typical |
| Anxious | Chest pain |
| Hyperventilating | Risk factor - HTN |
| Non-radiating pain | Pain feels pressure-like and tight (MD) |
| Sharp pain | Nausea and vomiting |
| Pain on chest palpation | Diabetes |
| Pain with coughing | Nausea and vomiting |
| Pain with deep breath | |
| Productive cough | |
| Chills for the last week | |
| No improvement with NTG | |
| Onset during sleep | |
| Headache | |
| Appears anxious | |
| Chest wall tenderness |
What happened in this case?
 The physician absolutely anchored on the atypical symptoms. He used the wrong mental algorithm; he was swayed by the cognitive bias of triage cuing; or he independently and inappropriately anchored on elements in the atypical list. From the deposition testimony, it is not clear which atypical symptom took him down the wrong path and caused the failure to diagnose. But looking specifically at the physician notes regarding the quality of the pain, the associated symptoms and the risk factors for CAD, the atypical nature of the presentation should not have altered his thought process. This patient needed continuing evaluation and admission or observation for further testing.
The physician absolutely anchored on the atypical symptoms. He used the wrong mental algorithm; he was swayed by the cognitive bias of triage cuing; or he independently and inappropriately anchored on elements in the atypical list. From the deposition testimony, it is not clear which atypical symptom took him down the wrong path and caused the failure to diagnose. But looking specifically at the physician notes regarding the quality of the pain, the associated symptoms and the risk factors for CAD, the atypical nature of the presentation should not have altered his thought process. This patient needed continuing evaluation and admission or observation for further testing.
When you look at cases like this in retrospect, it is easy to wonder how a board certified emergency physician could possibly have discharged this patient with a diagnosis of chest wall pain. Don’t discount the power of heuristics or the cognitive disposition to respond – in other words, human bias. The patient was 35-years-old, complained of a productive cough, and had worsening pain with cough and pain with palpation of the chest wall. She described the pain as sharp and she had reported intermittent chills; she had a normal ECG and initial troponin.
This case is presented in this issue in order to help practitioners avoid bias and recognize the pitfalls leading to this common failure to diagnose.
Have you experienced an interesting case recently? Share with The Sullivan Group and we'll review for potential future inclusion in our Clinicians Corner.