[5 MIN READ]
[5 MIN READ]
Before the COVID pandemic, the medical community in general, and physicians in particular, were dealing with and continue to deal with a pandemic of its own: Burnout. In 2019, burnout was categorized as a disease by the WHO. It is characterized as:
“…a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.”
There are 3 dimensions of burnout:
- Feelings of energy depletion
- Increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job
- Reduced professional efficacy
If someone is suffering from any of these dimensions, they are considered burned out. Unlike depression or other mental health diagnoses, burnout is mostly an occupational phenomenon. This is particularly important when examining the effects of COVID on burnout. If any of the factors that lead to burnout is impacted in a negative way, then the impact on burnout is transferrable to the physician. In simple terms:
If A (Causes) leads to B (Burnout), and C (COVID) increases the magnitude of A, then the outcome, B, is also increased.
So let me divide the rest of this blog into three parts: A, B, and C.
A: Causes
Review of the literature identifies several factors that contribute to burnout. When Christina Maslach developed the Maslach Burnout Inventory, she described the three main causes of burnout:
- Unmet expectations
- Lack of control
- Insufficient rewards
From: Maslach C, Zimbardo PG. Burnout: The Cost of Caring. 2003. Malor Books. Lost Altos, CA.
According to a Medscape survey, the translation of these categories in medicine in terms of measurable and identifiable factors have been proven/shown in numerous studies; they include the following:
According to the AMA and research conducted by Medscape, the following risk factors impact burnout:
- Working too many hours: 3% increase each additional hour
- Taking night or weekend call: 3%-9% each shift
- Performing work-related tasks at home: 2% each hour
- Having a work-home conflict: 200%-250%
- Practicing in certain specialties – ER, IM: 300%
- Working in private practice: 20%
- Receiving incentive pay: 130%
- Feeling like a cog in the wheel
- Using computerized physician order entry or enduring other clerical burdens: 29%
- Scrutiny, evaluations, lawsuits, increasing demands
 Other causes of burnout are linked to leadership or the lack of it. In 2015, Tait Shanafelt in a landmark study showed:
Other causes of burnout are linked to leadership or the lack of it. In 2015, Tait Shanafelt in a landmark study showed:
- “…Mayo has demonstrated the importance of front-line leadership on the well-being and professional satisfaction of physicians.
- For every point upward on a 60-point scale, there was 9% greater staff satisfaction and 3.3% less burnout.
- At the department and division level, 11% of the variation in burnout and 47% of the variation in satisfaction with the organization was explained by the Leader Index of the chairperson.”
From: Shanafelt, T et al. Impact of Organizational Leadership on Physician Burnout and Satisfaction. Mayo Clinic Proceedings. 4/2015 90(4): p. 432-440 4. Swensen, S., et al.
The expression goes: “People quit their bosses, not their jobs.” We know now that poor leadership makes for higher burnout.
- Pressure “is where the outcome is important to you, it is uncertain, and you are accountable and judged for the results. You must deliver the goods or suffer dire consequences. It adversely impacts cognitive success, downgrades behavioral skills, we perform below our capability, often camouflaged and is continually increasing.” Weisenger H, Pawliw-Fry JP. (2015) Performing Under Pressure: The Science of Doing Your Best When It Matters Most. New York, NY: Crown Business.
- Personal characteristics include perfectionism, idealism, certain personality types, racism, and being self-critical.
- Last but not least, physicians lose their purpose and the ability to fulfill our needs. When they are not able to emotionally connect to their patients, demonstrate clinical competency, and be professionally autonomous, they become burned out.
B: Burnout
According to psychologists Herbert Freudenberger and Gail North (Jan. 2019), burnout goes through a 12-stage model:
- Compulsion to prove oneself
- Working hard – with an inability to switch off
- Neglecting basic needs – lack of sleep, lack of healthy eating, lack of social interaction
- Displacement of conflicts – problems are dismissed
- Revision of values – values are skewed, friends and family dismissed, hobbies irrelevant
- Denial of emerging problems
- Withdrawal – social life small or nonexistent
- Odd behavioral changes – changes in behavior obvious to friends and family
- Depersonalization – seeing neither self nor others as valuable
- Inner emptiness
- Depression
- Burnout syndrome – includes mental and physical collapse; medical attention required
How these 12 stages manifest are effectively summarized in one of several landmark studies by Tait Shanafelt.
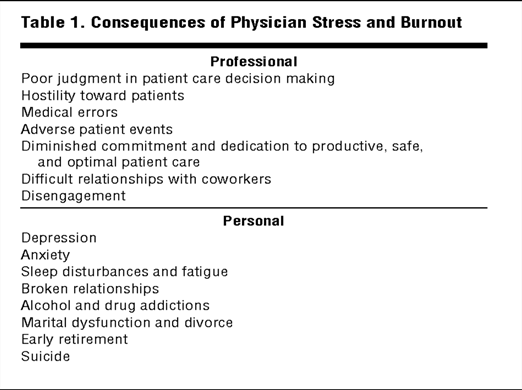
Adapted from: Balch CM, Freischlag JA, Shanafelt TD. Stress and Burnout Among Surgeons: Understanding and Managing the Syndrome and Avoiding the Adverse Consequences. Arch Surg. 2009;144(4):371-376. doi:10.1001/archsurg.2008.575.
C- COVID
When COVID hit the healthcare industry, it impacted all of the causes listed above in the following way:
- It increased uncertainty.
- It cut jobs and decreased pay.
- It jeopardized the provider and his or her family.
- There was even less controlling of the disease, the public, and the potential threats.
- It created an even bigger distance between providers and their patients.
- It increased the pressure of practicing medicine.
- It negatively impacted expectations.
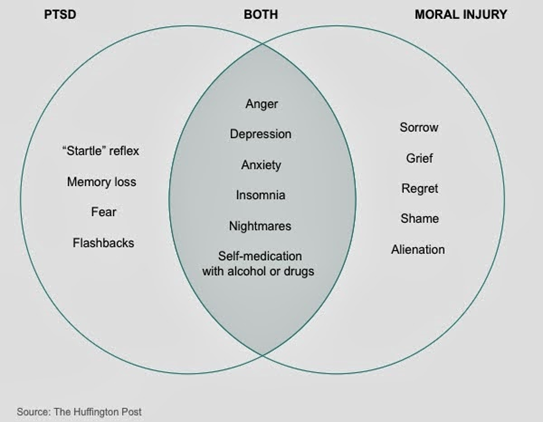
COVID also increased moral injury. “Moral injury refers to an injury to an individual's moral conscience and values resulting from an act of perceived moral transgression, which produces profound emotional guilt and shame, and in some cases also a sense of betrayal, anger, and profound ‘moral disorientation.’”
Physicians have had to practice medicine below the normal standards of care; they were allowed to do so. Whereas it might have been the safer approach, it impacted them in a negative way because they were providing subpar care, and that caused them to be morally injured. According to psychologists, moral injury intersects with PTSD in certain aspects, as diagrammed below.
Burnout and COVID: The MAACU Effect
The literature has shown that COVID has:
- Magnified the factors leading to burnout.
- Accelerated the pathophysiology of burnout.
- Amplified the burnout signs and symptoms.
- Created new signs and symptoms.
- Uncovered hidden signs and symptoms.
Dealing with one pandemic was problematic for the healthcare industry. Adding COVID to it is really stressing physicians. More physicians are thinking of leaving the profession, and fewer are thinking of entering it in the first place. While most of the focus has been to protect this workforce from COVID, the chaotic scenes from the beginning of the pandemic, the toll it is taking and has taken and will continue to take, the plethora of its signs and symptoms, the uncertainties facing it now, and the unknowns of the future remind us of the more deadly burnout pandemic. On average, one physician commits suicide on a daily basis. The last thing burnout needs is something to make it worse.
This sacred profession is under attack. Thankfully, there is a tremendous increase in awareness and the future looks brighter now than it ever did. For that and so much more, many thanks, prayers, and love are shared with each and every physician. Thank you for all that you do. This world is a much better place because of your dedication, resilience, tenacity, love of human life, and your unrelenting promise to help others.