[8 MIN READ]
[8 MIN READ]
I recently reviewed the bare-bones of what EMTALA is and highlighted recent studies of EMTALA investigations.
In this installment, I have summarized nine recently settled EMTALA cases in which monetary penalties were levied by OIG against the hospital that serve to illustrate the factors responsible for alleged violations.
Emergency Medicine EMTALA Violations
Failure to screen for EMC
An Alabama hospital entered into an $80,000 settlement agreement with OIG in 2018 regarding allegations of failure to provide an adequate medical screening examination and stabilizing treatment. The patient was a 35-year-old male with chest pain and shortness of breath who presented to the ED accompanied by his girlfriend.
The patient requested to see a physician and became belligerent when a nurse asked him why. That led to the patient being escorted out of the ED by security. Several minutes later, the patient returned to the ED.
This time, the patient's girlfriend drove up to the ambulance bay and reported that the patient had suffered a seizure and was lying in her truck. She was informed by staff that they would not help get the patient out of the truck. In addition, the security guard told her she had to leave.
The patient's girlfriend then took him to another hospital, where he was pronounced dead within 20 minutes of his arrival.
Failure to stabilize a patient with EMC
 A Tennessee hospital entered into a $25,000 settlement agreement with OIG regarding allegations that it failed to stabilize an EMC for a 58-year-old patient who presented to the ED for blurred vision and dizziness. After failing to provide an appropriate EMC, an ED nurse directed the patient to a local eye doctor and failed to provide medical treatment to stabilize the patient's EMC, a cerebral infarction.
A Tennessee hospital entered into a $25,000 settlement agreement with OIG regarding allegations that it failed to stabilize an EMC for a 58-year-old patient who presented to the ED for blurred vision and dizziness. After failing to provide an appropriate EMC, an ED nurse directed the patient to a local eye doctor and failed to provide medical treatment to stabilize the patient's EMC, a cerebral infarction.
Hospital failed to accept transfer of a patient with EMC
A Tennessee Hospital “B” entered into a $40,000 settlement agreement with OIG regarding allegations that it failed to accept an appropriate transfer. A 13-year-old presented to Hospital “A” complaining of testicular pain. An ultrasound indicated no evidence of blood flow in the right testicle.
The ED requested that Hospital “B” accept the patient for transfer. However, the on-call urologist at Hospital “B” refused to accept the transfer of the patient, recommending instead that the patient be transferred to another facility.
OIG alleged that Hospital “B” declined to accept the appropriate transfer when it had both the capability and capacity to stabilize the patient's emergency medical condition (EMC).
Inappropriate transfer of a patient with EMC
 A Georgia hospital entered into a $52,414 settlement agreement with OIG in 2018 regarding allegations that it inappropriately transferred a patient to another hospital.
A Georgia hospital entered into a $52,414 settlement agreement with OIG in 2018 regarding allegations that it inappropriately transferred a patient to another hospital.
The patient, a 58-year-old woman, arrived at the ED of Hospital “A” by private vehicle complaining of left-sided pleuritic chest pain and abdominal pain.
An ED physician examined the patient and noted that her abdomen was diffusely firm with hypoactive bowel sounds. The patient's blood samples revealed that her lactic acid and bleeding and clotting time were elevated. The patient's chest X-ray showed a large amount of intraperitoneal air under the right diaphragm, which suggested bowel perforation.
The ED physician discussed the patient's condition with the on-call surgeon, who recommended that the patient be transferred to Hospital “B” where she had undergone a dilation and curettage procedure two days earlier. Hospital “B” agreed to accept the transfer and asked that the patient be air-lifted to its facility.
Three hours and forty-seven minutes after her arrival at Hospital “A,” the patient was transferred to Hospital “B” in critical condition. Upon arrival at Hospital “B,” the patient was in septic shock and on the verge of respiratory collapse. Even after receiving emergency surgery to repair the bowel perforation, the patient's condition continued to worsen, and she died later that day.
Obstetric-Related EMTALA Settlements
Here are a few illustrative case summaries of recent obstetric-related EMTALA settlements in which monetary penalties were levied by the OIG against the hospital:
Failure to provide medical screening exam and stabilize an obstetric patient in active labor
A North Carolina hospital entered into a $40,000 settlement agreement with OIG in 2017 regarding allegations that it failed to provide an adequate medical screening examination (MSE) and stabilizing treatment for a woman who presented to the ED in labor with her third child. The patient was discharged a little over one hour after she presented.
The OIG alleged that the hospital did not properly examine the patient or check the progress of her labor before she was discharged. The patient drove home and immediately gave birth to her child at home.
Failure to appropriately transfer an obstetric patient
An Ohio hospital entered into a $50,000 settlement agreement with OIG in 2018 regarding allegations that it failed to provide an adequate MSE and transfer for a patient.
The patient, a 33-week pregnant woman, presented to Hospital “A” complaining of leaking fluids, pelvic pain and vomiting. An ED nurse told the patient that the hospital did not have an obstetrician on site and that the patient could either start treatment at Hospital “A” and be transferred later, or that her male companion could drive her immediately to Hospital “B” where her obstetrician practiced.
After being told this, the patient left Hospital “A” by private vehicle to Hospital “B,” a thirty-minute drive. Hospital “A” never provided the patient or her unborn child an MSE and failed to transfer this patient who had an EMC. At Hospital “B,” the patient underwent an emergency C-section and delivered a male infant without a heartbeat. The receiving hospital's efforts to revive the infant were unsuccessful.
Psychiatric-Related EMTALA Cases
Here are summaries of recent representative psychiatric-related EMTALA cases in which monetary penalties were levied by the OIG against the hospital as part of settlement agreements:
Failure to provide adequate MSE and stabilizing treatment for a psychiatric patient
 An Iowa hospital entered into a $100,000 settlement agreement with OIG in 2017 regarding allegations that it failed to provide an appropriate psychiatric screening examination or stabilizing treatment for three patients who presented to the emergency department (ED) when an on-call psychiatrist was available:
An Iowa hospital entered into a $100,000 settlement agreement with OIG in 2017 regarding allegations that it failed to provide an appropriate psychiatric screening examination or stabilizing treatment for three patients who presented to the emergency department (ED) when an on-call psychiatrist was available:
- A woman presented to the ED complaining of depression and suicidal thoughts but was later discharged with instructions to follow up with her primary care physician.
- A child presented to the ED following violent outbursts but was later discharged with instructions to follow up with his primary care physician.
- A man presented to the ED stating his mind was "disturbed," but later eloped from the ED into single-degree weather wearing paper scrubs while his discharge was processed. His body was found about 300 feet from the hospital; the cause of death was attributed to hypothermia.
Inappropriate discharge of a psychiatric patient
A Missouri hospital entered into a $100,000 settlement agreement with OIG in 2017 regarding allegations that it discharged patients with unstabilized EMCs, albeit pursuant to the hospital’s policy that stated if a patient had a blood alcohol level (BAL) above 100, the patient was given to local law enforcement and taken to jail.
For example, a 41-year old man presented to the ED after attempting suicide by overdose. The patient was depressed, had a history of psychiatric problems, and had recently been admitted for electroconvulsive therapy. The patient's BAL was 288, and he was discharged into the custody of local law enforcement and taken to jail.
The next day, the patient was seen by a counselor in jail and then released from custody. The patient returned to the hospital that evening after again attempting suicide by overdose. The patient had slurred speech, was lethargic, and had a flat affect; he was admitted to the intensive care unit in guarded condition.
Failure to stabilize and treat psychiatric patients: a batch of 36 incidents
A South Carolina hospital entered into a $1,295,000 settlement agreement with OIG in 2017 regarding allegations that the hospital violated the Emergency Medical Treatment and Labor Act (EMTALA) in 36 incidents. In these incidents, individuals presented to the hospital’s ED with unstable psychiatric EMCs.
Instead of being examined and treated by an on-call psychiatrist, and despite empty beds in its psychiatric unit to which the patients could have been admitted for stabilizing treatment, the patients were involuntarily committed and kept in the ED for between 6 and 38 days each. The following is an example of one such incident.
A patient presented to the ED via law enforcement with psychosis and homicidal ideation and was involuntarily committed. The patient did not receive psychiatric examination or treatment by available psychiatrists and was not admitted to the psychiatric unit for stabilizing treatment. Instead, the patient was kept in the ED for 38 days; at one point she was seen by a psychiatrist from another facility who was familiar with her condition. The psychiatrist prescribed a variety of medications for agitation. The patient eventually was discharged home.
EMTALA Violation Commonalities
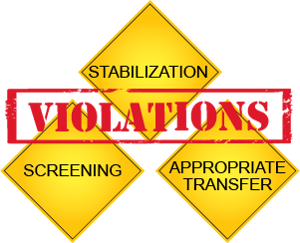 These alleged EMTALA violations do not hinge on the interpretation of an esoteric clause in the EMTALA statute. Rather, what they have in common is the violation of one or more basic requirements of EMTALA – screening, stabilization and appropriate transfer.
These alleged EMTALA violations do not hinge on the interpretation of an esoteric clause in the EMTALA statute. Rather, what they have in common is the violation of one or more basic requirements of EMTALA – screening, stabilization and appropriate transfer.
The circumstances of obstetric- and psychiatric-related EMTALA violations tend to be somewhat more complicated than strictly medical or trauma cases. The added dimension to OB and psychiatric cases is one of consultation; when presented with an OB or psychiatric emergency patient, the ED physician should consult an obstetrician or psychiatrist early and often to enlist their assistance in screening and stabilization.
Acknowledging that OB and psychiatry services are not available in all hospitals, the next priority is timely and appropriate transfer once appropriate screening and stabilization measures have been undertaken. All members of the hospital care team – ED physicians and nurses, on-call physicians, and administrators – must be experts in the fundamentals of EMTALA and refresh their competence on a regular basis.
These publicly available summaries of EMTALA settlements are stark reminders that the basic requirements of EMTALA continue to be violated. Obstetric and psychiatric patients present unique challenges in the quest to meet the basic EMTALA requirements of screening, stabilization and appropriate transfer.
Hospitals and healthcare professionals should continue efforts to educate themselves regarding the requirements of EMTALA and the potential ramifications of non-compliance.
Related Content
- 10 Medical-Legal Basics Every Provider Must Know
- EMTALA for On-Call Physicians
- Informed Consent Form Process & Documentation
Reference
U.S. Department of HHS, Office of Inspector General. Civil Monetary Penalties and Affirmative Exclusions. Available at: https://oig.hhs.gov/fraud/enforcement/cmp/cmp-ae.asp. Accessed February 5, 2019.