 [7 MIN READ]
[7 MIN READ]
As heightened U.S. maternal morbidity and mortality rates gain national attention, AWHONN and ACOG, as well as state perinatal quality collaboratives, notably California, have emphasized that hospitals need to focus on improving outcomes with specific attention to the leading causes of maternal mortality.
The RSQ® Assessment – Obstetrics provides the framework for the creation of a comprehensive obstetrics safety program within your organization, as well as the foundation for an obstetric culture of safety surrounding the key drivers of maternal mortality and morbidity.
Why Use the RSQ® Assessment – Obstetrics?
We created the RSQ® Assessment – Obstetrics as part of an obstetrics and perinatal safety initiative in 2014 with one of the largest healthcare organizations in the country to measure the level of compliance with specific oxytocin safety indicators and how compliance impacted both maternal and neonatal outcomes.
The study, as published in articles and white papers (links to AJOG and case study) and presented at several professional conferences, reshaped the culture of oxytocin safety within over 300 hospitals nationwide. The organization continues to use the assessment tool in all hospitals, placing significant value on the data collected, improved outcomes achieved, and sustainable safety practices.
What is it?
The RSQ® Assessment – Obstetrics is an intrapartum safety assessment tool that strategically promotes evidence-based and standardization practices focused on both maternal and fetal safety. Key elements of the assessment align with national perinatal initiatives to reduce maternal morbidity and mortality. While intrapartum care is highlighted, it also has antepartum and postpartum indicators specific to leading causes of maternal death. The tool measures whether best practices are being implemented by staff and providers.
In addition to oxytocin administration and management safety practices, the assessment tool templates highlight:
- reduction of primary C-section
- documentation for shoulder dystocia
- hypertensive crisis
- postpartum hemorrhage
- maternal and neonatal outcomes
Each template allows pertinent data capture fostering the development of meaningful quality projects that ultimately translate into outcome improvements. This tool provides easy data abstraction from the patient medical record and offers real-time data analysis in an organized easy-to-read and understandable format. Data transparency sets the stage for purposeful analysis and team-driven desire for optimal improvement. Interdisciplinary clinical excellence can be conquered and sustained with data-driven quality improvement initiatives that align with specific key perinatal issues.
 Results can be applied to numerous elements of clinical practice that support the highest safety standards. The on-going capture of pertinent data also allows for the consideration of publications and showcasing of facility improvement and benchmark attainment.
Results can be applied to numerous elements of clinical practice that support the highest safety standards. The on-going capture of pertinent data also allows for the consideration of publications and showcasing of facility improvement and benchmark attainment.
Designed for the entire perinatal team, this assessment tool helps track and improve the performance of all who have a stake in promoting perinatal safety on your unit, including physicians, nurses, midwives, obstetric managers, directors, and educators. Engaging the entire perinatal team is a critical step in encouraging a culture of safety and facilitating process improvement.
How to start a program?
Assessment Planning Process
- Design your program with TSG. Our Obstetric Customer Success Team will assist you through the process of creating a safety program at your facility including set-up, on-boarding, and orientation. We recommend an initial focus on one or two components that align with your current unit initiatives. Each unit has their own unique needs and we will work with you to create an assessment process that will target your goals.
- Select your unit’s perinatal safety team leaders. These folks are your team champions for the assessment and considered your go-to people for assessment questions and concerns. Not only will they serve as your unit’s assessment resource person, they will also be the link to the TSG They will be designated as the assessment administrators and have access to all the collected data and reported results, as well as any selected scores that may be applied.
- Meet with TSG for Orientation. Your team leaders will confirm which safety assessments your organization will implement to reach your unit’s goals. You will select audit criteria specific to your targeted initiatives. Sample size will be determined. Time frames will be established for data entry and rapid data analysis. PDSA (Plan, Do, Study, Act) style formats are encouraged. While we recommend a quarterly review process, your team might choose monthly, quarterly or more frequently depending on preference and how you implement action plans.
How do I implement the assessment?
- Determine record selection process. Patient record selection process is reviewed and HIPAA protections implemented.
- Select auditors/reviewers. Auditors should be experienced OB staff that have vested interest in improving unit safety and are committed to correct data entry. It is helpful if auditors are AWHONN Fetal Heart Monitor (FHM) certified or NCC certified, so that there is clinical competence regarding data collection. Other certifications in obstetrics would also be useful; RNC-Inpatient OB
- TSG will provide auditor/reviewer orientation. We will provide orientation to each selected OB assessment template and demonstrate site navigation and data entry with opportunity for questions and answers to ensure understanding of tool functionality. Auditor/reviewers need to have a comfort level with the site navigation and data entry process prior to starting.
- Auditors/reviewers become familiar with the audit criteria, audit questions and site navigation. Auditors should familiarize themselves with the audit questions and requirements and how to access the selected records. They should take some time to do a trial entry of data. Once they are comfortable, data entry may begin. Reviewers will become adept at data entry and their time commitment will decrease as they become proficient.
How will my organization benefit from using the RSQ® Assessment – Obstetrics?
- Promotes on-going assessment of key perinatal and obstetric initiatives
- Provides ability to measure whether goals were achieved
- Provides ability to measure both unintended harm and lack of harm on your OB unit
- Provides ability to readily identify gaps in safety and quality improvement opportunities
- Promotes provider and staff situational alertness/awareness to key safety issues
- Promotes timely response to strategic safety issues
- Provides a process for evaluation of quality care as it relates to leading causes of maternal morbidity and mortality
- Promotes standardization of process and reduces variability of process while promoting consistency and sustainability
- Evaluates strategic communication practices on your unit
- Provides ability to assess data on multiple levels; hospital/medical group/MD/Midwife/ and allows for comparison to other nationally set benchmarks
- Provides data transparency facilitating team camaraderie and team approach to safety
- Provides data-driven opportunity for quality improvement
- Provides formal process for evaluation of maternal-fetal outcomes
- Provides opportunity for shared-outcome process
- Promotes and supports the 4 domains of the ACOG AIM Bundles; readiness, recognition and prevention, timely responsiveness and on-going reporting and evaluation
- Mitigates risk, decreases unintended catastrophic consequence
What are some examples of action plans generated from the data?
- Work with staff to readily identify tachysystole and respond in a timely fashion before it causes unintended fetal consequence
- Work with providers to achieve scope of understanding for protocols that allow adequate time frames for second stage labor as determined by maternal-fetal status
- Implement of a checklist specific to a safety initiative; for example, a pre-oxytocin checklist or oxytocin in-use checklist
- Educate an entire OB unit on culture change regarding promotion of vaginal delivery
- Educate an entire OB unit on the leading causes of maternal mortality, what gaps in care exist on the unit and what needs to be implemented to correct these gaps
- Implement safety algorithms specific to an area of weakness
- Engage providers to regularly view and compare their C-section rates with peers and against national benchmarks, provide a specific learning path to achieve reduction of individual C-section rates
- Implement new process specific to improving notification of OB stat team.
What reports are available to management?
While management has access to several reports, below we highlight two critical action plans that can be implemented using reports available.
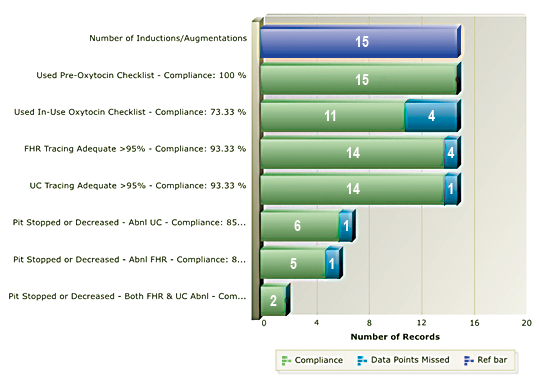
This first report below addresses 3 issues regarding oxytocin use: 1. Use of checklist prior to administration; 2. Use of checklist during administration, and 3. Appropriate response to FHR tracings during oxytocin use.
The resulting action plan involved education regarding the importance of checklist use, including the opportunity to prevent potentially unsafe situations and early recognition of errors and omissions that lead to unintended consequences. The facility also provided guidance on a standardized workflow. Scores improve as staff understand the critical steps of oxytocin safety and follow the standardized process.
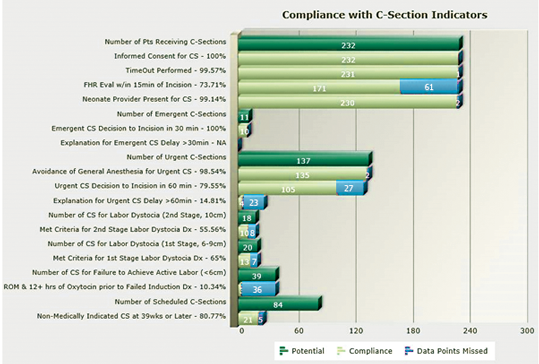
This second report analyzes compliance with C-Section Indicators, supporting discussions surrounding management of labor with the transformative goal of reducing C-Sections. As a result, this facility was able to improve upon decision to incision time frames for C-sections. It also brought transparency to issues of first and second stage labor dystocia and ACOG’s suggested criteria for failed inductions.
Summary
Optimization of safe obstetric practice requires commitment and team support. The RSQ® Assessment – Obstetrics provides the framework to help you build a sustainable obstetrics safety program by helping you recognize areas that require urgent attention, identify culture change opportunities, and offer tangible solutions for implementation of quality measures that will ultimately lead to improved outcomes and reduced fear of litigation.
Contact us if you’re interested in viewing a demonstration of the RSQ® Assessment – Obstetrics, including individualized physician reports, facility reports, and ideas for implementation of an aggressive interdisciplinary safety program for your organization.


