In a previous posting, “The Ultimate Loss Prevention Strategy: 4 Key Areas of Allocating Your Risk Management Budget,” we highlighted the importance of addressing Diagnosis-Related Adverse Events. As an extension of that article, Dr. Tom Syzek and I provide further detail for justifying that recommendation and the recent data surrounding diagnostic errors, after which we will outline three key attributes of successful initiatives that have led to positive results.
Quick Review of the Data
In 2015, the HMD (Health and Medicine Division - formerly IOM) released the report “Diagnostic Error in Health Care,” which indicates that the majority of adverse events that lead to litigation stem from a diagnosis-related event.
The 2014 CRICO Comparative Benchmark System (CBS) National Landscape Analysis reveals that diagnosis-related allegations accounted for the highest total incurred cost in their loss history at just over $1 billion (4,184 MPL cases from 1/1/09-12/31/13). Furthermore, the majority of diagnosis-related cases result in high-severity injuries (death, permanent grave, permanent major, or permanent significant) and account for over 80% of the financial losses.1
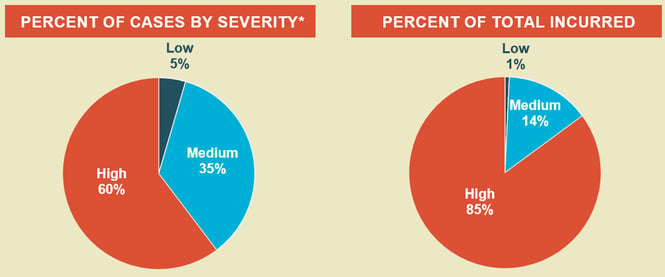 Copyrighted by and used with permission of The Risk Management Foundation of the Harvard Medical Institutions, Inc., all rights reserved.
Copyrighted by and used with permission of The Risk Management Foundation of the Harvard Medical Institutions, Inc., all rights reserved.
The claims data shows that diagnostic errors represent a significant area of exposure to patient injury and that litigation helps provide an awareness. However, Dr. Allen Kachalia’s analysis of missed and delayed diagnosis malpractice claims (published in the Annals of Emergency Medicine) advances the discussion and identifies common fact patterns.
A Quick Summary of Dr. Kachalia’s Findings 2
- Cognitive errors were involved in 96% of the cases:
- Mistakes in judgment (87%)
- Lack of technical competence or knowledge (58%)
- Lapses in vigilance or memory (41%)
Good News: You Can Make a Positive Impact
 Up to this point, you might be feeling that this article feels leans towards the “glass half empty” side of the spectrum. Fortunately, several organizations have had success in avoiding adverse events and litigation related to diagnostic errors. With that in mind, let’s review some key attributes of successful initiatives that have led to positive results.
Up to this point, you might be feeling that this article feels leans towards the “glass half empty” side of the spectrum. Fortunately, several organizations have had success in avoiding adverse events and litigation related to diagnostic errors. With that in mind, let’s review some key attributes of successful initiatives that have led to positive results.
Proactive
This particular attribute speaks more to the philosophy, framework and design of the loss prevention initiative. While peer review activities are helpful, merely relying on this “reactive” approach may not reveal the clinical risk exposures prior to an adverse event taking place. Consider defining a profile of the most common missed/delayed diagnosis claims associated with a particular specialty. From that profile, perform an ongoing, prospective analysis of your clinician’s practice, regardless of the patient outcome.
For example, analyze the last 30 medical records from chest pain patients over 40 years of age that presented to your Emergency Department and measure the frequency that clinicians appropriately assess and document the clinical elements related to Acute Myocardial Infarction, Pulmonary Embolism, and Thoracic Aortic Dissection (e.g., radiation of pain, location of pain, etc.). Augmenting your peer review process with this prospective analysis could reveal clinical risk exposures before they become an adverse patient safety event.
Clinically Relevant
 Ensuring that the content of your patient safety initiative is clinically relevant not only leads to the positive changes in clinical practice that you hope to achieve, but it also ensures the successful adoption of the program. Many organizations implement an online training (CME/CE) program for their clinicians. This is an important component to have in place for a strong loss prevention program. However, the content of the curriculum has to be viewed as truly meaningful to your clinician’s practice. We have found that clinicians respond very favorably to case-based, clinical scenarios that provide specific recommendations for improving practice and/or documentation. In that same vein, any prospective analysis of their practice must measure the clinical elements that actually impact the diagnostic process. Building an initiative around the “soft science” aspects of the clinical environment will likely frustrate clinicians and will not lead to meaningful positive changes in clinical practice.
Ensuring that the content of your patient safety initiative is clinically relevant not only leads to the positive changes in clinical practice that you hope to achieve, but it also ensures the successful adoption of the program. Many organizations implement an online training (CME/CE) program for their clinicians. This is an important component to have in place for a strong loss prevention program. However, the content of the curriculum has to be viewed as truly meaningful to your clinician’s practice. We have found that clinicians respond very favorably to case-based, clinical scenarios that provide specific recommendations for improving practice and/or documentation. In that same vein, any prospective analysis of their practice must measure the clinical elements that actually impact the diagnostic process. Building an initiative around the “soft science” aspects of the clinical environment will likely frustrate clinicians and will not lead to meaningful positive changes in clinical practice.
Sustainable
Regardless of the industry, implementing an error reduction program has to be enduring, and healthcare is no exception. When you factor in attrition rates and the human desire to revert back to old habits, it is critically important to build an initiative that can become part of the organization’s culture. Relying simply on “onsite consultations” or even one individual’s ability to impact everyday clinical practice appears to be a losing proposition in the long run. If you have invested in a proactive strategy that is clinically relevant, you should expect to see impact in your loss history over time, which contributes to the sustainability of the initiative. That said, continuously proving a negative can be a tough proposition and it requires discipline to maintain the course.
Resources
1 CRICO Comparative Benchmark System: National Landscape. 2014.
2 Kachalia et al. Missed and delayed diagnoses in the emergency department: A study of closed malpractice claims from 4 liability insurers. In the February 2007 Annals of Emergency Medicine 49(2), pp. 196-205.